Post Cardiac Arrest for Infants & Children with Glasgow Coma Scale (GCS) < 8 after Initial Resuscitation
NEUROLOGIC MONITORING
- Clinical – obtain baseline neurologic examination without muscle relaxants
- Routine nursing neurovitals assessment hourly
- Routine head of bed elevated 20-30° with head in neutral midline position
- Initial neuroimaging after discussions with neurology and neuroradiology
- Follow-up imaging typically MRI at 72 hours in consultation with neuroradiology
HEMODYNAMIC SUPPORT
- Monitoring: arterial line - for routine indications
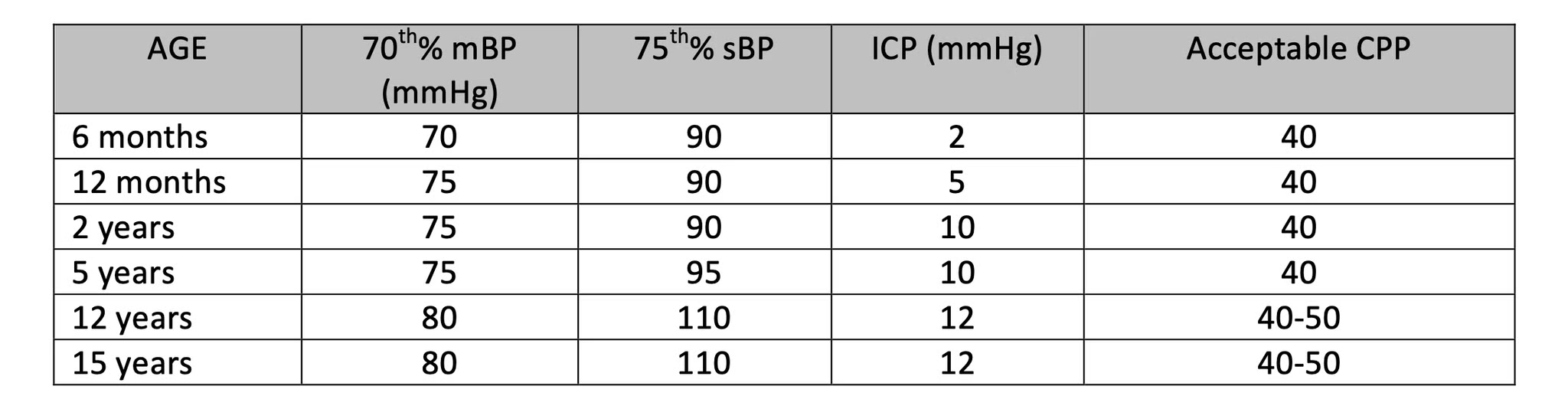
- Maintain mean arterial pressure upper end of normal based on normal age ranges
- Inotropes as required/fluids as required
- Cardiac echo for usual indications
- Depending on the circumstances, cardiology consult to help determine etiology of
cardiac arrest (eg. cardiomyopathy) Persisting shock, consider the reversible causes 5H’s/5T’s (5H: hypovolemia,
hypothermia, hyperkalemia, hypoxemia, hydrogen ion (acidosis) 5T: toxins, tamponade, tension
pneumothorax, thrombosis – coronary/pulmonaryVentilation & Oxygenation
- Intubated/mechanically ventilated
- Maintain ETCO2 35-40mmHg
- Wean FiO2 to maintain arterial saturations >=94-99%
- Protective lung ventilation
- Consider neuromuscular blockade to facilitate ventilation/oxygenation management
Fluid & Electrolytes
All patients with brain injury (anoxic or traumatic) are at risk for disordered sodium regulation. Early detection of sodium abnormalities is essential to maintaining serum sodium within target range and preventing secondary brain injury.
- D5W 0.9%NaCl at 70% maintenance initially
- Foley catheter and hourly urine output measurement for 48 hours
- Monitor serum electrolytes and blood gases every 6 hours for 48 hours – serum Na to maintain 140 or above
- Initial labs should include liver “function” and coagulation screen
- Maintain serum glucose 5-8mmol/L
- Notify PICU physician if urine output is < 0.5cc/kg/hour, > 4cc/kg/hour in a single hour, or > 2.5cc/kg/hour for more than three hours
Temperature Control
- Monitor core temperature – esophageal
- Normothermia 36-36.8C (external cooling if necessary) 48 hours and reassess
- Regular acetaminophen 15mg/kg every 6 hours NG/NJ
- Review every 24 hours
- Consider neuromuscular blockade to facilitate temperature control
Sedation & Analgesia
- Every effort should be made to allow clinical examination each morning by the medical and nursing teams by reducing sedation or discontinuing muscle relaxants
- Follow routine procedure for pain and sedation
- Initiate routine analgesia and sedation based upon the clinical condition, unless contraindicated or neurologic condition dictates otherwise
Seizures
- EEG within first 24 hours of admission and continuous EEG monitoring if indicated (electrographic seizures captured or EEG shows high potential for electrographic seizures)
Spinal Precautions for Near Hanging Patients
- Semi-rigid cervical collar (Aspen) maintained until cervical spine cleared (see C-05-07-60737 Cervical Spine Clearance: Pediatric Trauma Patient (healthcarebc.ca), refer to Cervical Spine Clearance Protocol for Children with GCS ≤8 (page 4 of link)
- CTA head and neck within 24 hours of admission to exclude major vessel and laryngeal injuries, depending on the clinical situation. If cervical spine CT is normal, cervical spine precautions can be discontinued and the collar removed
Nutrition
Dependent on the clinical condition of the patient:
- If hemodynamically unstable, maintain NPO – NG to free drainage
- Consider initiating feeds once hemodynamic stability has been achieved
- Commencing within 24 hours of admission if lactic acidosis has cleared and minimal inotropic support
- If gastric paresis persists beyond 48 hours, a jejunal feed tube should be placed
Close monitoring required during initiation of enteral feeds to avoid hyponatremia
Post Cardiac Arrest Care Checklist Link
Components of Post- Cardiac Arrest Care [Internet]. Available from: https://cpr.heart.org/-/media/CPR-Images/CPR-Guidelines-Images/Part-4-Pediatric-Basic-and-Advanced-Life-Support/PCAC_Checkllst_200814.jpg?h=877&w=700&hash=50E892F188226B26EEF820F31B8EA0D3.