Equipment
- Appropriate device to provide NIPPV
- Appropriate type and sized mask interface
- Appropriate securing head gear for mask
- Appropriate circuit
- Appropriate humidification device to provide patient with humidified gas mixture
- Circuit tubing
- Oxygen tubing (optional)
- Oxygen saturation monitor
- Sterile water for inhalation
BCCH Respiratory Care Steering Committee. NON-INVASIVE POSITIVE PRESSURE VENTILATION: INITIATION AND MANAGEMENT AT BCCH [Internet]. 2023. Available from: https://shop.healthcarebc.ca/phsa/BCWH_2/BC%20Children%27s%20Hospital/C-0506-12-62066.pdf
Set Up & Management
*Download guideline for details
- PERFORM hand hygiene and DON personal protective equipment (PPE)
- DETERMINE and OBTAIN appropriate NIPPV delivery device and appropriate sized
mask and headgear for NIPPV - CONNECT all circuit tubing to the NIPPV device
- CONNECT NIPPV device to power source and ensure the power cable is securely
connected to the NIPPV device - ATTACH oxygen if required. Set up according to the device manual
- TURN ON NIPPV device and set appropriate mode and settings. Perform leak check and
confirm pressure remains stable - ENSURE humidification is set-up appropriately for the device. Ensure the humidification device is TURNED ON
- SUCTION patient (if required) before placing mask on patient’s face
- ATTACH the circuit tubing to the patient’s mask. CONFIRM there is flow before
applying the mask to the patient’s face - ATTACH the mask to the patient’s face and secure headgear
- COMPLETE a site-to-source check once headgear is secure and device is on the
patient - ASSESS the patient and perform a site to source check of the NIPPV system Q3H and
as needed.
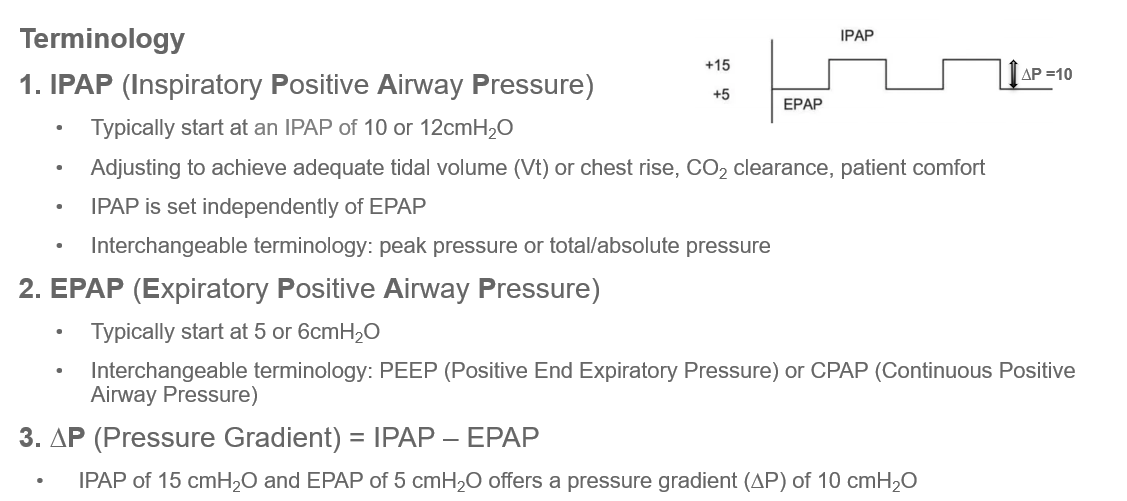
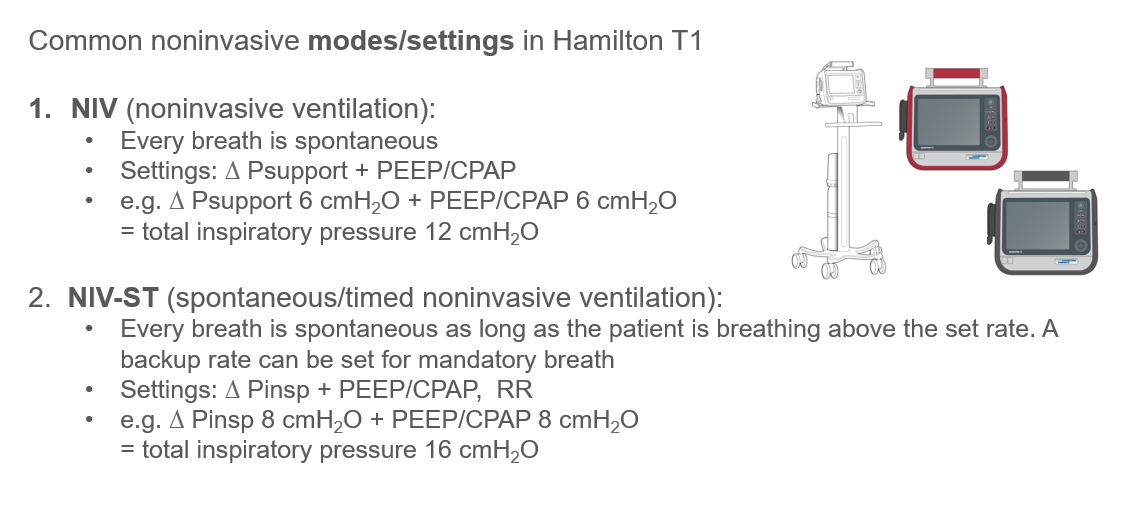
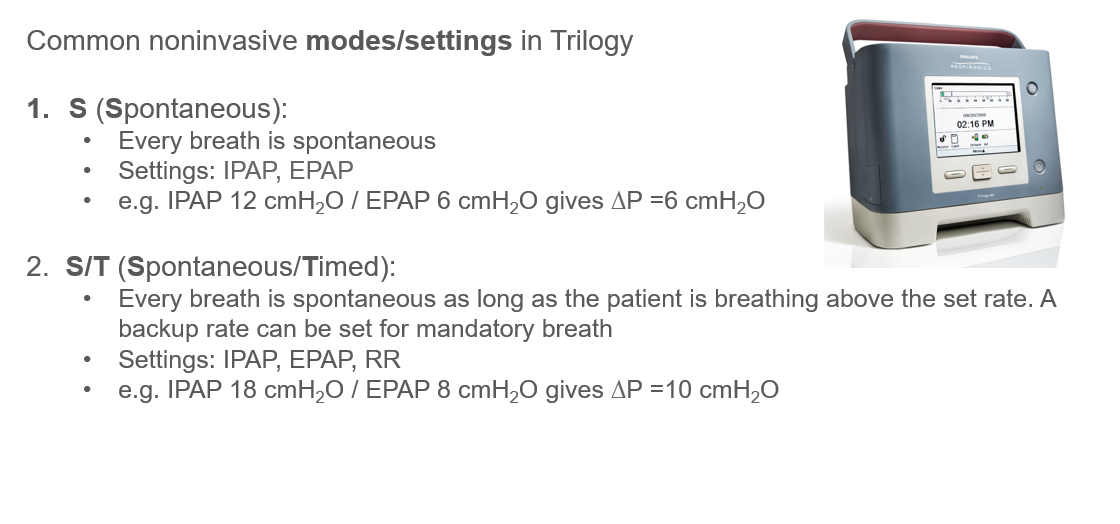
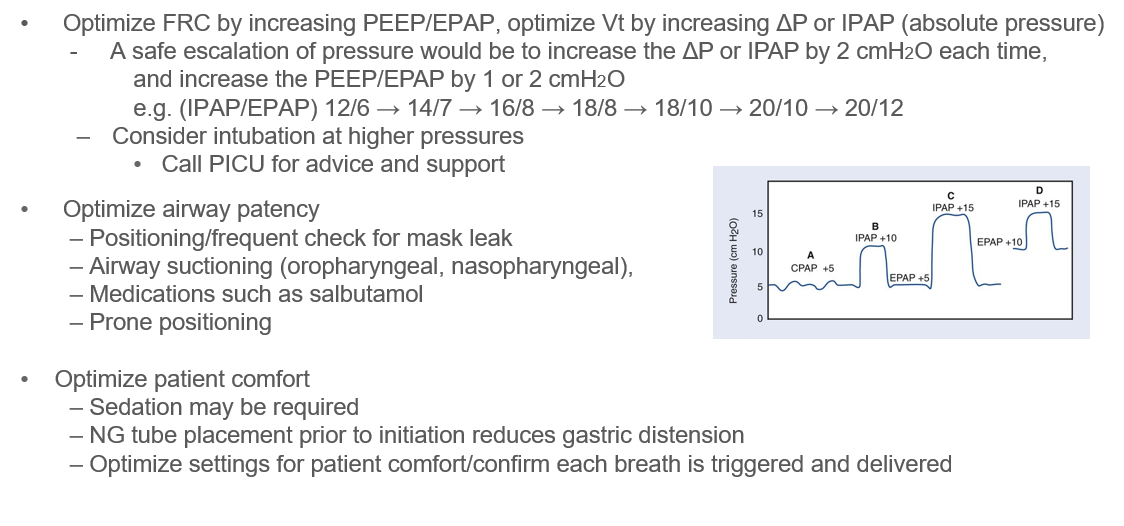
Settings on BiPAP
References:
BiPAP: Bilevel Positive Airway Pressure
FRC: Functional Residual Capacity
Vt: Tidal Volume
BC Children’s Hospital PICU Physicians RT 2025. Available from:
Medication Administration
Important considerations should be noted when administering medication to patients requiring respiratory support, including NIPPV
Best practice: MDI + Spacer
- Pre oxygenate as needed
- Remove BiPAP mask
- Administer MDI + spacer with mouthpiece/mask to deliver medication
- If MDI + spacer is not available, consider a large volume chamber or vibrating mesh nebulizer (VMN). If not available, a small volume nebulizer is an option.
Note: VMNs provide superior dose delivery compared to SVNs
If the patient cannot tolerate being off non-invasive ventilation for medication delivery via MDI + spacer, consider VMN.
Dual-Limb Circuits (ie. Hamilton T1 ventilator, Servo-U ventilator, etc.)
- Place the VMN on the dry side of the humidifier pot.
Use a non-vented patient interface.
Image
Single-Limb Circuits (ie. Trilogy ventilators, Breas Vivo 45LS ventilator, etc.)
- Place the VMN between the patient interface and exhalation port.
Use a non-vented patient interface.
Image
Ari, A. et al. (2010) Influence of Nebulizer Type, Position, and Bias Flow on Aerosol Drug Delivery in Simulated Pediatric and Adult Lung Models During Mechanical Ventilation. Available at: https://rc.rcjournal.com/content/respcare/55/7/845.full.pdf.
Branconnier MP, Hess DR. Albuterol Delivery During Noninvasive Ventilation.
Hassan, A. et al. (2017) In-vitro/in-vivo comparison of inhaled salbutamol dose delivered by jet nebulizer, vibrating mesh nebulizer and metered dose inhaler with spacer during non-invasive ventilation. Available at: https://www.tandfonline.com/doi/full/10.1080/01902148.2017.1282993.