Traumatic Brain Injury (TBI)
Pediatric Considerations
- Children have larger head-to-body size ratios (higher incidence of head trauma), thinner cranial bones (increased risk of skull fractures), and unfused sutures (better initial tolerance of increased intracranial pressure)
- Pediatric brains have increased water content and decreased myelination making children more susceptible to shear injuries (e.g., diffuse axonal injury) and cerebral swelling
- Consider abusive head trauma in infants and young children
TREKK. Severe Head Trauma. 2022. Available: Trekk - Severe Head Injury
Assessment
- Apply spinal motion restriction when indicated
- Once need for advanced trauma care is identified, refer and organize transport early after stabilization to optimize outcomes
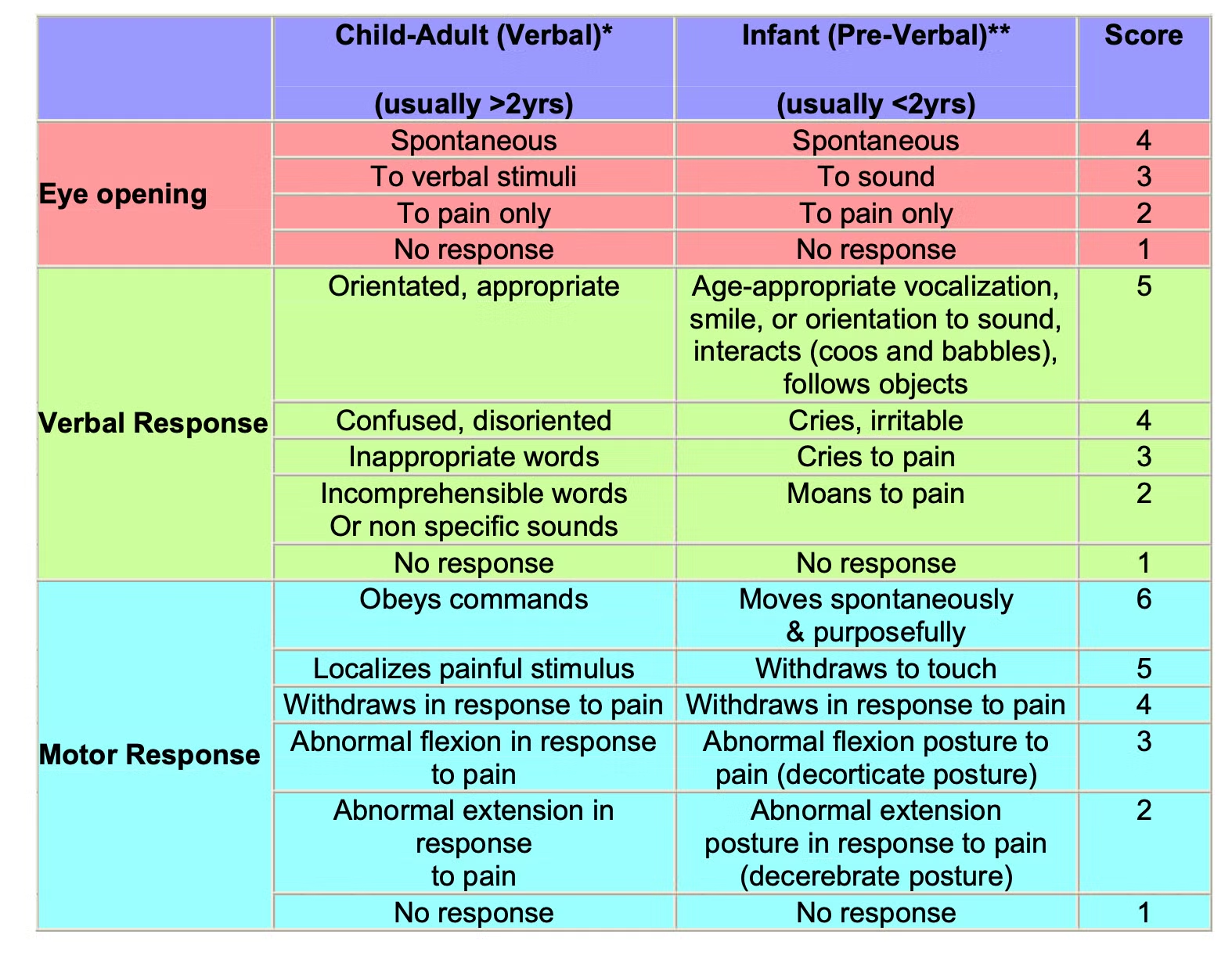
- Use the modified Glasgow Comma Scale (GCS) for Infants and Children to assess and document neurological status in preverbal children
- Assume multisystem injury in all children presenting with significant head trauma due to mechanism of injury and smaller size/unique anatomy
- Manage airway of children with severe Traumatic Brain Injury (TBI) prior to transport.
- Recognize intracranial hypertension and cerebral herniation by:
- Progressive obtundation
- Unilateral pupillary dilatation
- Cushing’s triad (hypertension, bradycardia, abnormal respiration)
BCCH Child & Youth Health Policy and Procedure Manual. APPENDIX A: MODIFIED GLASGOW COMA SCALE (GCS) FOR INFANTS AND CHILDREN [Internet]. Available from: https://shop.healthcarebc.ca/phsa/BCWH_2/BC%20Children%27s%20Hospital/C-05-14-62116.pdf
Treatment
TREATMENT
The main goal of treatment of TBI is to prevent secondary brain injury by maintaining cerebral perfusion while minimizing increased intracranial pressure.
Cerebral Perfusion Pressure (CPP) = Mean Arterial Pressure (MAP) – Intracranial Pressure (ICP)
- Neuroprotective measures with expedient transfer are critical to optimizing outcome
- Avoid hypoxia and hypotension with effective airway and hemodynamic support. These 2 factors contribute most to secondary brain injury
- Aim for normothermia and normocapnia (ETCO2 35-40). Hyperventilation is reserved for herniation
Management of Intracranial Hypertension/ Cerebral Herniation
- Hyperventilation to reverse pupillary dilation, reverse Cushing’s Triad, and/or ETCO2 of 30-35.
- Raise head of bed to 30 degrees and loosen cervical collar or provide manual in-line stabilization.
- Hyperosmolar agents
- Mannitol 20% (0.5–1 g/kg, 2.5–5 mL/kg IV over 15 min) or
- NaCl 3% (2.5–5 mL/kg IV over 15 min) - Airway protection while spinal motion restriction is maintained
- Neurosurgical consultation for hematoma evacuation or decompression craniectomy
TREKK. Severe Head Trauma. 2022. Available: Trekk - Severe Head Injury
Drs. Peter Skippen, Ash Singhal, Mandeep Tamber, Mary Connolly, Linda Huh. MANAGEMENT OF TRAUMATIC BRAIN INJURY IN CHILDREN WITH GCS < 8. [Internet]. 2021. Available from: https://shop.healthcarebc.ca/phsa/BCWH_2/Pharmacy,%20Therapeutics%20and%20Nutrition/C-05-07-62754.pdf.